A report of our mapping exercise with other researchers from Scripps Gerontology Center to define the boundaries of Palliative Care and End of Life Choices.

In 2016, a small group of researchers associated with Scripps Gerontology Center at Miami University noticed a common interest that kept coming up in regular meetings—the present state and future of palliative care. We then formed a Palliative Care/End of Life Choices Research Interest Group associated with Scripps, where Gerontologists, Sociologists, Designers, Economists, and experts from other backgrounds share their research and thinking in this area. Group meetings have sparked some enlightening conversations and opportunities for research, but they have also highlighted the complex nature of palliative care—most notably, the question:
What are the boundaries of palliative care?
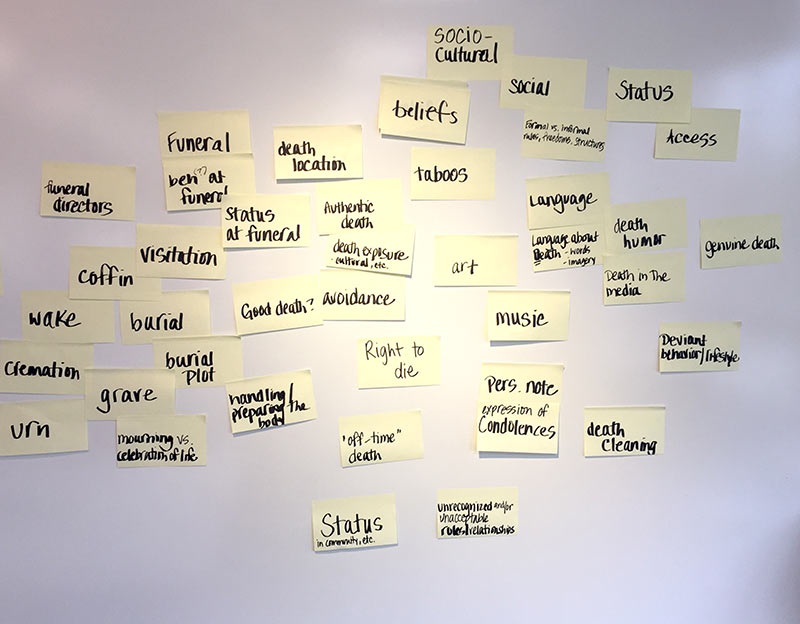
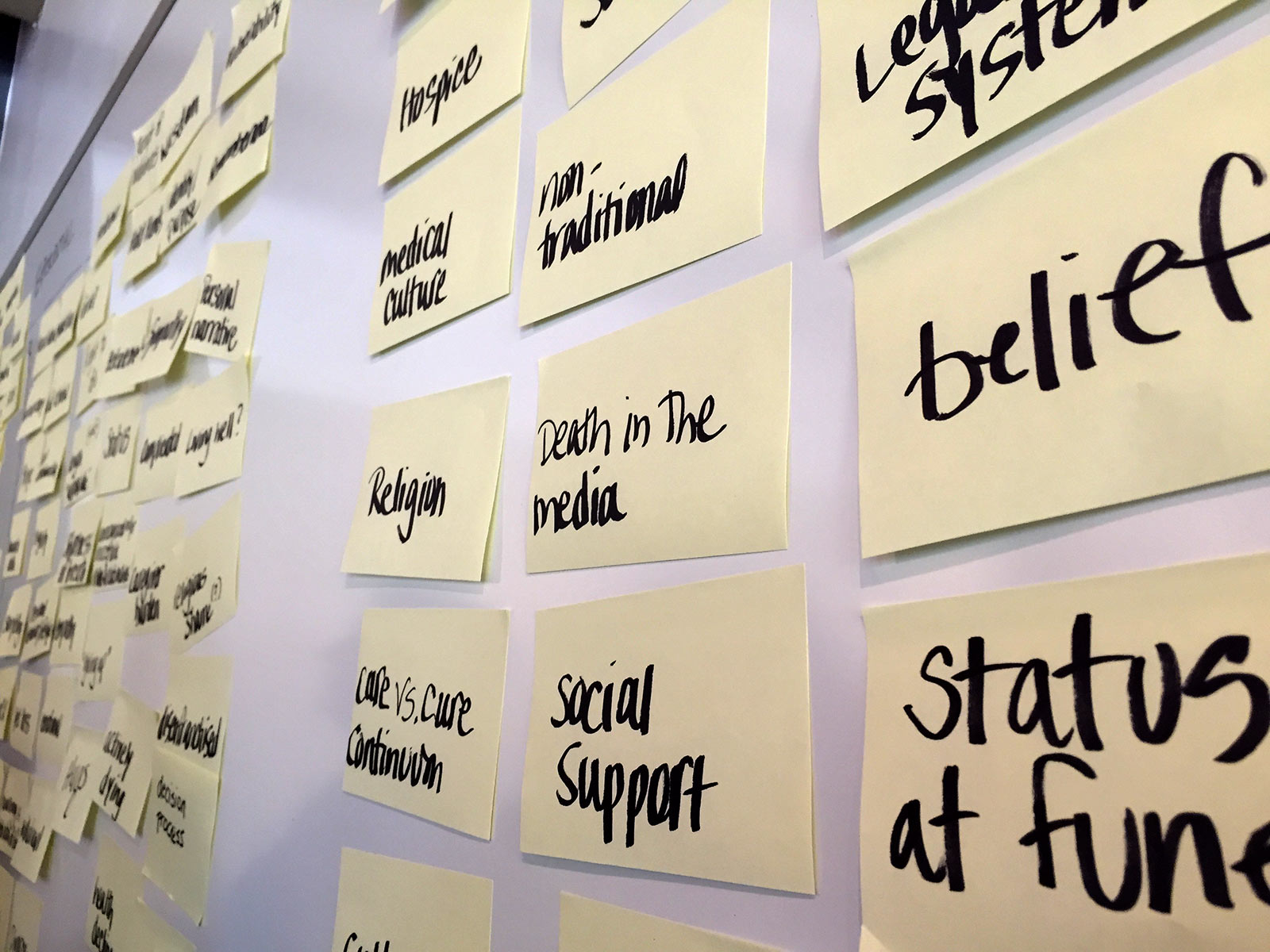
On October 12 and 19, 2017, members of the Palliative Care/End of Life Choices Research Interest Group got together in the xdMFA Design Studio at Miami University in Oxford, Ohio, for concept mapping exercises designed to get some answers. Both Jennifer Heston and Dennis Cheatham, members of the Living Values research project, are associated with Scripps and led the collaborative exercise. While our Research Interest Group did not expect that we could cover every corner of palliative care, we felt that by working together, we could map many aspects that could inform research collaborations, initiatives, as well as a literature review. During the October 12 session, our group generated as many aspects of palliative care as possible in one hour using a fluid concept development process. In the October 19 session, things started to take shape as these aspects were arranged as a concept map.
Aspects and Boundaries Come in All Shapes and (Invisible) Sizes
During the October 19 session, our process for generating and categorizing aspects of palliative care was driven by three discrete qualities of palliative care: formal, experiential, and systems. These classifications were broad enough to spark conversation between about ten participants.
Formal Aspects
Tangible, real items and people are involved in palliative care. Even the most minor things can have profound impacts on people involved in palliative care. Formal aspects included anything that could be touched, observed, or tangibly manipulated, regardless of size. The team generated factors including DNRs, (Do-Not-Resuscitate Order), doctors, breathing machines, pets, heirlooms, donated organs, and hospitals.
Experiential Aspects
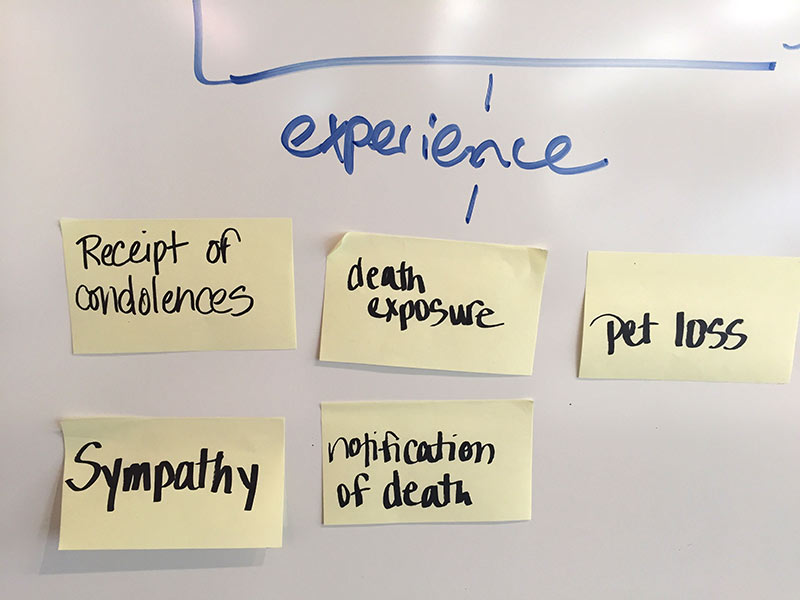
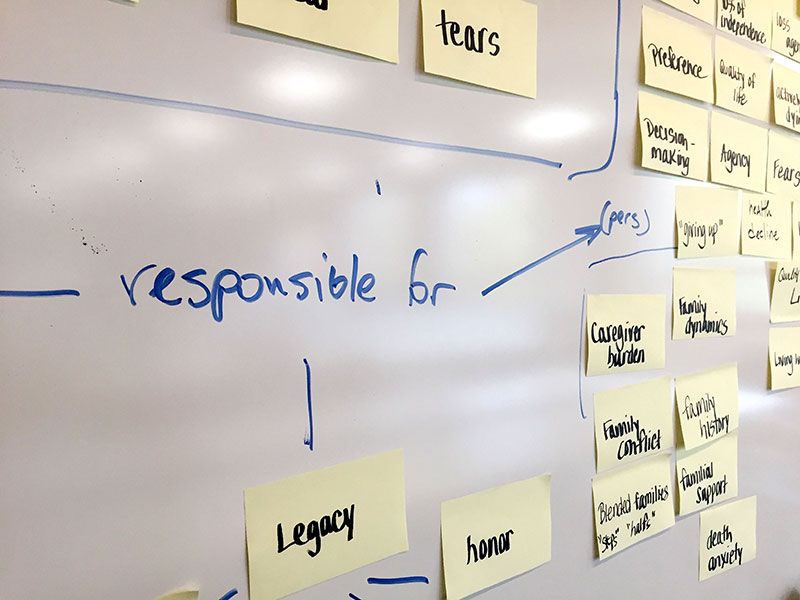
Palliative care involves people, services, and interactions. The group generated experiential aspects like hugs, empathy, status, prayer, fear, holding hands, and preference. While these may not be tangible, they are fundamental factors that impact choices at large and small scales.
Systems Aspects
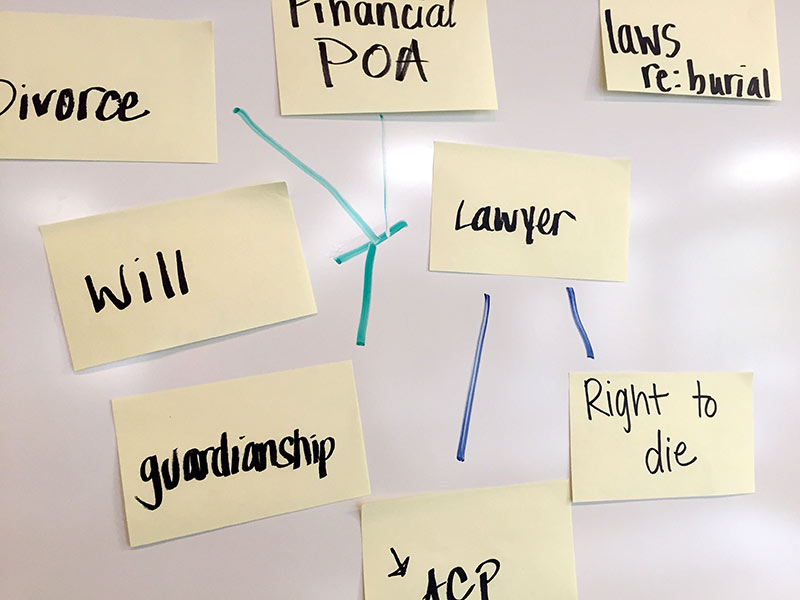
Based on the experiences of the Research Intrest Group members, palliative care and end-of-life choices don’t occur in a vacuum—they are interconnected. The issue often involves systems connected with other systems. Systems-related aspects were generated during the group’s process, including the legal system, familial support, Hospice, spirituality, and education.
Next Steps
Our group is reconvening in December to discuss the concept map and how it can fuel the next steps. Based on the discussion that has followed, it’s folly even to think palliative care has “boundaries.” However, themes have started to emerge from the activity, and researchers are beginning to define projects our work will fuel. Our Living Values team is excited to be part of work that has no boundaries.
Here are a few images from the October 19 activity.